How to Handle a Declined ACC45
Issue
An ACC45/Claim, Appointments billed to ACC under that Claim, have been declined by ACC. What should be done?
Solution
If ACC declines a Claim, then the Claim Type needs to be updated from ACC to Private or Insured, depending on who it will now be billed to.
Follow the steps below to update the appointment details:
-
Edit the condition that the ACC45 is related to and update the Claim Type (in this example to Insured)


-
If there are existing appointments for this Condition, you will need to modify them and change the Service Type as required.
For Example, if changed to an Insured Condition, the Client may still be charged the surcharge. Or the Insurer may be covering the appointment charge and the surcharge, which would be billed to them in a new Insurer Schedule.
See ACC Has Declined a Single Treatment Within an ACC45.

-
Reject the item from the schedule.
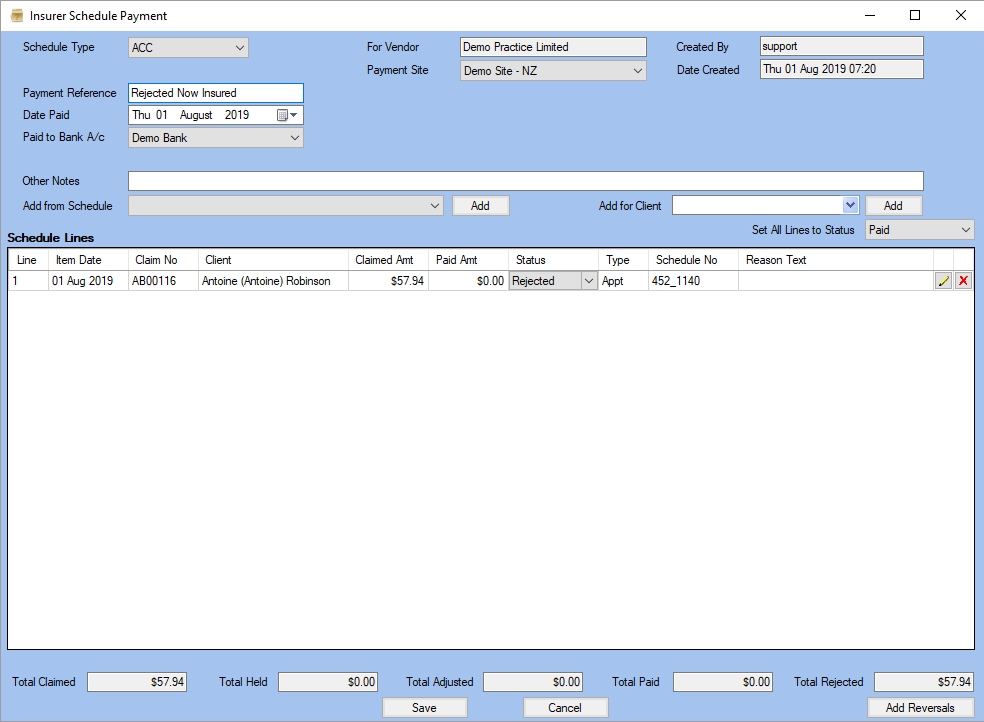
Note: If any appointments have already been batched in schedules to ACC, you can reject them from those schedules in advance. Alternatively, you can wait until you receive rejection notification and reject them at that point.
-
This is how the appointment would look once the steps are followed. In this example the insurer is paying the surcharge also. This appointment is now ready to be included in a new Insurer Schedule.

Note: Clinicians on EPN Contracts and Hand Therapists have a 50 appointments allowance and their conditions do not expire. Clinicians on Regulation Contracts have an allowance of 16 appointments and their conditions have an expire date.